At thirty-one, Emma Goidel, who successfully became pregnant after six rounds of Intrauterine insemination (IUI) and one round of invitro fertilization (IVF), filed a class-action lawsuit against Aetna. This action on how infertility coverage is biased against LGBTQ people calls attention to the unique family planning challenges faced by members of the LGBTQ community. The lawsuit claims “Aetna’s discriminatory policy is an illegal tax on LGBTQ individuals that denies the equal rights of LGBTQ individuals to have children.” While coverage kicks in immediately for heterosexual couples, resulting in zero out-of-pocket cost for treatment, the policy’s discriminatory rules require LGBTQ patients to pay thousands of dollars out of pocket before their coverage kicks in.
It is clear fertility is facing a tipping point for the modern family. IVF was first introduced 40 years ago. Since this revolutionary advancement in treatment, assisted reproductive technology (ART) has created a new fertility landscape filled with promise for those seeking to start or grow their family through non-traditional methods. Yet, access to revolutionary treatments have been out of reach for many. LGBTQ individuals face increased barriers to accessing fertility care. Typically, these families do not meet the definitions of “infertility” that would qualify them for covered associated health care plans. Transgender individuals undergoing gender-affirming care may also not meet the criteria for “iatrogenic infertility” that would qualify them for covered fertility preservation.
After a half-dozen attempts and one successful pregnancy, Emma and her spouse were denied coverage for treatment under Aetna’s Student Health Policy for Columbia University. The couple was told that because Emma had not yet met Aetna’s classification of infertility, treatment was denied.
The policy defines infertility as “not becoming pregnant after 12 months of regular, unprotected heterosexual sex—or 12 months of therapeutic donor insemination.” This timeframe is reduced if the person who is trying to get pregnant is 35 or older. Once this requirement is reached the health plan will cover IVF and IUI.
Emma appealed and continued to file claims with Aetna, but the outcome remained the same. Emma expressed how the exclusive policy “really feels like a queer tax” after the couple paid over $45,000 out-of-pocket for treatment.
Just two days after the lawsuit was filed, Aetna released a statement, recognizing that Emma was improperly denied coverage and they will work to change the policy.
Employees Want Options For Pursuing Parenthood
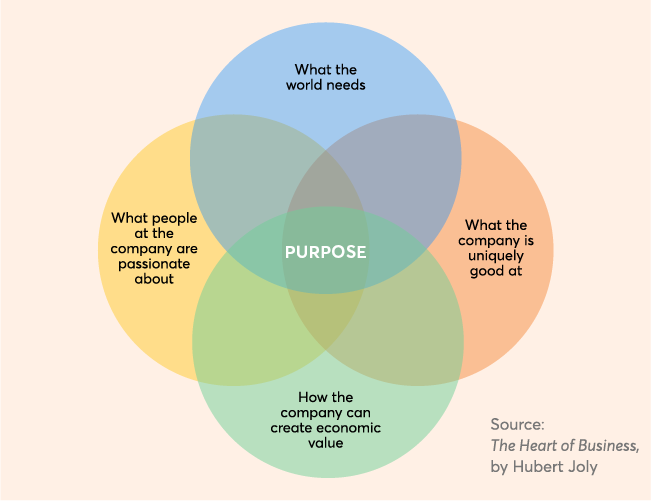
Employees who are seeking healthier outcomes and lower healthcare costs deserve a flexible suite of benefits tailored to support their unique needs. Sadly, as demonstrated in this case, many family planning benefits are constructed and maximized for families led by two heterosexual partners. Indeed, infertility benefits coverage has not kept up with contemporary families who are pursuing parenthood in diverse families headed by single parents; unmarried couples; and lesbian, gay, bisexual, or transgender people. These outdated and discriminatory benefits are creating inaccessible medical treatment.
In the absence of insurance coverage, fertility care is out of reach for many people. Most people seeking fertility treatment, pay for the services themselves, with totals reaching well over $10,000 in some cases. The average cost of an IVF cycle in the US is $15,000.
Human resource managers should advocate for their employees and make sure that every individual is represented and has access to inclusive benefits packages. The spotlight on this lawsuit has created an opportunity to put same-sex couples on the same footing as other couples who are trying to start a family.