The Wellable Blog
The Power of Wellness through Rewards and Recognition
Learn how wellness rewards and recognition can motivate your teams, improve workplace well-being, and build healthy habits.
The Power of Wellness through Rewards and Recognition
Learn how wellness rewards and recognition can motivate your teams, improve workplace well-being, and build healthy habits.
How to Make a Budget-Friendly Wellness Plan
Learn how to make a budget-friendly wellness plan that boosts engagement, well-being, and productivity using free resources and low-cost ideas.
Is an Annual Wellness Plan or a One-time Challenge Right for Your Organization?
Discover the benefits of an annual wellness program vs. a one-time challenge and determine which approach drives lasting behavior change and engagement.
20 Ways to Celebrate Work Anniversaries in 2025
Discover 20 creative ways to celebrate work anniversaries that make employees feel valued, appreciated, and motivated to stay for years to come.
15 Ways to Celebrate Heart Month in the Workplace
Discover 15 fun activities for heart health awareness to promote heart health at work, raise awareness, and inspire employees with actionable initiatives.
22 Employee Engagement Ideas
Explore actionable strategies to boost employee engagement, increase productivity, and foster a motivated, loyal workforce for long-term business success.
What is the Best Time of Year to Launch a Corporate Wellness Program?
Learn when to roll out a corporate wellness program to capitalize on seasonal trends and enhance employee participation.
Seven 2025 Winter Wellness Challenges For Employees
Explore seven winter wellness challenge ideas for employees to boost mindfulness, inspire healthy habits, and improve well-being during colder, darker months.
White Paper: Best Practices to Maximize Employee Engagement Through Incentives
Discover data-driven insights from Wellable and ThrivePass customers on top incentive strategies to maximize engagement in wellness programs.
How to Support Employees Navigating Seasonal Affective Disorder (SAD)
Explore how to support employees with Seasonal Affective Disorder through empathetic leadership, flexible arrangements, and actionable workplace strategies.
The Implications Of The 2024 Election For Employer Health Plans
Explore how the 2024 election could impact employer health plans, including potential policy changes, emerging healthcare trends, and preparation strategies for organizations.
The Best Corporate Wellness Apps To Support Mental Health In The Workplace
Explore the best corporate wellness apps to support employee mental health and well-being, including features that maximize engagement and effectiveness.
Women In The Workplace 2025: Research And Trends
Explore top trends and challenges for women in the workplace in 2025, and discover ways to make progress toward true equity.
The Ultimate Guide To Peer-To-Peer Recognition At Work
Explore how peer-to-peer recognition boosts engagement, retention, and morale with practical tips to create a supportive, appreciation-driven workplace culture.
Employee Recognition Ideas
Explore employee recognition ideas that boost morale, strengthen culture, and motivate your team, including meaningful, non-monetary gestures.
How To Pick The Best Reward Structure For Your Wellness Program
Learn how to choose a reward structure for your wellness program that aligns with company goals, fits your budget, and motivates employees to participate.
7 Alternatives To The Body Mass Index (BMI)
Discover effective BMI alternatives including body roundness index, waist-to-hip ratio, body fat scales, and more for a more accurate health evaluation.
How To Support Employees With Chronic Illness
Learn how to proactively support employees working with chronic illness through flexible policies, compassionate leadership, and inclusive workplace practices.
Wellness Incentives: How To Create An Impactful Employee Rewards Program
The secret to wellness program engagement lies in offering engaging rewards. Learn how to create a wellness incentives program that boosts participation and promotes long-term health.
How To Build Employee Confidence At Work
Confidence building at work requires support, recognition, and trust from employers. Learn how to build confidence in employees for innovation and engagement.
How to Make a Budget-Friendly Wellness Plan
Learn how to make a budget-friendly wellness plan that boosts engagement, well-being, and productivity using free resources and low-cost ideas.
Is an Annual Wellness Plan or a One-time Challenge Right for Your Organization?
Discover the benefits of an annual wellness program vs. a one-time challenge and determine which approach drives lasting behavior change and engagement.
15 Ways to Celebrate Heart Month in the Workplace
Discover 15 fun activities for heart health awareness to promote heart health at work, raise awareness, and inspire employees with actionable initiatives.
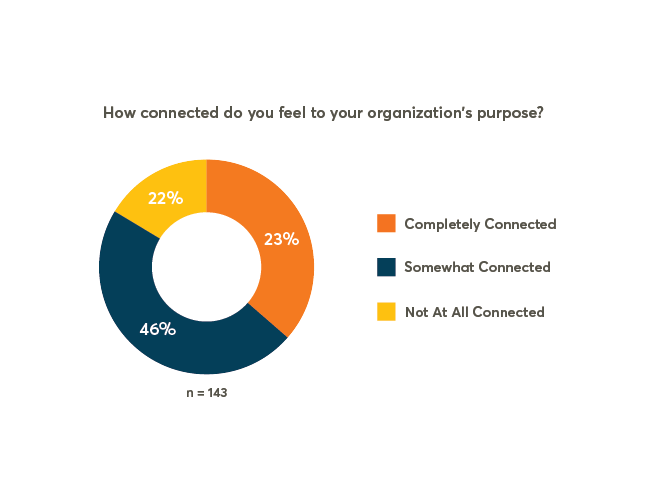
Pulse Check: 20% Of Employees Not Connected To Their Organization’s Purpose
Though employees are looking for meaningful jobs, many feel disconnected from their organization’s purpose. Explore why missions aren’t resonating with workers and learn what employers can do to better harness the power of purpose.
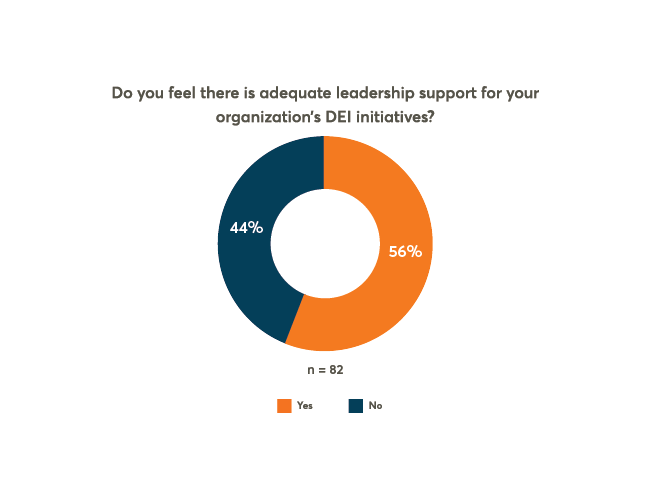
Pulse Check: 44% Of Employees Feel There Is Not Enough Leadership Support For DEIB
While most organizations have implemented DEIB strategies, employee perception of leadership support is low. Find out why and how to fix it.
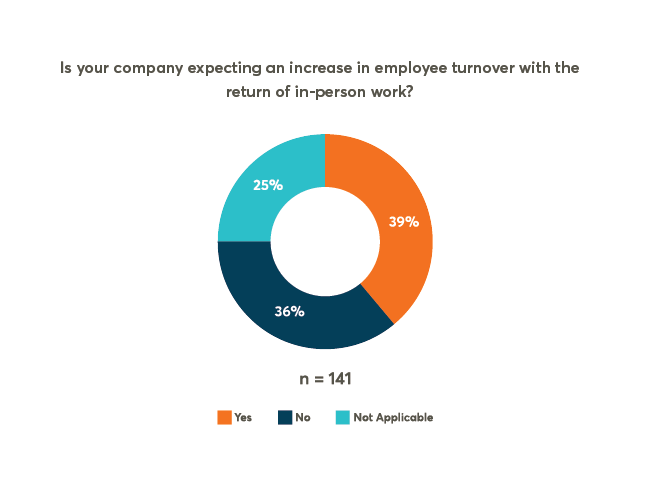
Pulse Check: Will The Return To In-Person Work Exacerbate The ‘Great Resignation’?
With resignation rates near their all-time highs, employers question whether their return-to-office plans will make matters worse. Check out these five tips for retaining talent during the transition back to in-person work.
20 Ways to Celebrate Work Anniversaries in 2025
Discover 20 creative ways to celebrate work anniversaries that make employees feel valued, appreciated, and motivated to stay for years to come.
22 Employee Engagement Ideas
Explore actionable strategies to boost employee engagement, increase productivity, and foster a motivated, loyal workforce for long-term business success.
White Paper: Best Practices to Maximize Employee Engagement Through Incentives
Discover data-driven insights from Wellable and ThrivePass customers on top incentive strategies to maximize engagement in wellness programs.